Are you waking up to a sharp, stabbing pain in your heel? Have have you been diagnosed with Plantar fasciitis ? You’re not alone. Plantar fasciitis affects millions, making each step a painful challenge. But don’t worry, there’s hope. In this article, we will explore the causes, symptoms, and, most importantly, the treatment options available, including plantar fasciitis surgery.
If non-surgical treatments haven’t worked for you, surgery might provide the relief you need. Understanding what plantar fasciitis surgery involves and what to expect during recovery is crucial. We’ve also covered non-surgical treatments and preventive measures to help you get back on your feet pain-free.
By taking proactive steps and consulting with a specialist, you can manage plantar fasciitis effectively. Early intervention and proper management are key to preventing the condition from worsening.
Table of Contents
Understanding Plantar Fasciitis
Plantar fasciitis is a condition where the plantar fascia, a thick band of tissue running across the bottom of your foot, becomes inflamed. This tissue connects your heel bone to your toes, providing support for your foot’s arch. When the plantar fascia is strained, it can develop small tears, leading to pain and inflammation.
Causes and Risk Factors
Several factors contribute to the development of plantar fasciitis. Overuse and repetitive strain from activities like running or prolonged standing are common causes. Wearing shoes with inadequate support, having flat feet or high arches, and being overweight also increase the risk.
Symptoms
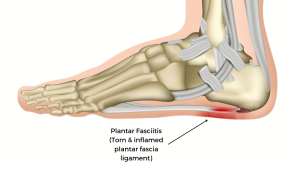 The hallmark symptom of plantar fasciitis is sharp heel pain, especially noticeable with the first steps in the morning or after rest. This pain often decreases as you move around but may return after long periods of standing or after exercise.
The hallmark symptom of plantar fasciitis is sharp heel pain, especially noticeable with the first steps in the morning or after rest. This pain often decreases as you move around but may return after long periods of standing or after exercise.
- Stiffness: Alongside pain, there may be noticeable stiffness in the heel and arch of the foot, making it difficult to walk or stand comfortably.
- Pain After Activity: While the pain may lessen during physical activity, it often returns with greater intensity after exercise or prolonged standing.
Progression of Symptoms
- Gradual Onset: The pain typically develops gradually over time. It might start as a mild discomfort and progressively worsen if not addressed.
- Localized Pain: The discomfort is usually localized to the heel, but in some cases, it can extend along the arch of the foot.
- Pain Flare-Ups: Symptoms can fluctuate, with periods of intense pain followed by times of relative comfort.
When to Seek Medical Advice
- Persistent Pain: If heel pain persists for more than a few weeks despite rest and home treatments, it is advisable to consult a plantar fasciitis specialist.
- Severe Pain: Intense pain that hinders your ability to perform daily activities should prompt a medical consultation.
- Associated Symptoms: If you experience swelling, redness, or tingling in the heel, it may indicate a more serious condition requiring professional evaluation.
Understanding the symptoms of plantar fasciitis is crucial for early diagnosis and effective treatment, helping to alleviate pain and restore mobility.
Diagnosing Plantar Fasciitis
 Accurate diagnosis of plantar fasciitis is essential for effective treatment. Consequently, a combination of physical examinations and imaging tests helps identify this condition and rule out other possible causes of heel pain.
Accurate diagnosis of plantar fasciitis is essential for effective treatment. Consequently, a combination of physical examinations and imaging tests helps identify this condition and rule out other possible causes of heel pain.
Physical Examination Techniques
- Patient History: The doctor will begin by asking about your symptoms, including the location and severity of the pain, and any activities that worsen or relieve it.
- Foot Examination: The doctor will check for areas of tenderness in your foot, especially around the heel and arch. This can help pinpoint the location of the pain and assess the extent of inflammation.
Imaging Tests
- X-rays: While X-rays do not show soft tissues like the plantar fascia, they can help rule out other conditions, such as fractures or bone spurs, that might cause similar symptoms.
- Ultrasound: This imaging technique can visualize the plantar fascia and detect thickening, tears, or inflammation.
- MRI: In more complex cases, an MRI may be ordered to provide detailed images of both the plantar fascia and surrounding tissues, ensuring a comprehensive assessment.

Differential Diagnosis
- Other Conditions: Several other conditions can mimic plantar fasciitis symptoms, such as Achilles tendonitis, tarsal tunnel syndrome, or a stress fracture. The doctor will consider these possibilities to ensure an accurate diagnosis.
- Gait Analysis: Observing how you walk can help identify any abnormalities or imbalances that might contribute to plantar fasciitis.
A thorough diagnosis helps in tailoring the most effective treatment plan, addressing the root cause of the pain, and promoting a quicker recovery.
Treatment Options for Plantar Fasciitis
 Effective treatment of plantar fasciitis involves a combination of home remedies, medical interventions, and, in some cases, surgical procedures. Therefore, understanding these options can help alleviate pain and promote healing.
Effective treatment of plantar fasciitis involves a combination of home remedies, medical interventions, and, in some cases, surgical procedures. Therefore, understanding these options can help alleviate pain and promote healing.
Home Remedies
- Rest: Limiting activities that aggravate the condition can reduce inflammation.
- Ice: Applying ice packs to the affected area for 15-20 minutes several times a day can help reduce pain and swelling.
- Stretching Exercises: Regular stretching of the calf muscles and plantar fascia can improve flexibility and relieve tension.
Over-the-Counter Medications
- Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation.
Physical Therapy
- Custom Exercises: A physical therapist can provide exercises to strengthen the muscles around the foot and ankle, improving stability and reducing strain on the plantar fascia.
- Manual Therapy: Techniques such as massage and mobilization can help relieve tension in the plantar fascia.
Custom Orthotics and Shoe Modifications
- Supportive Shoes: Wearing shoes with good arch support and cushioned soles can reduce stress on the plantar fascia.
- Orthotic Inserts: Custom-made orthotic devices can provide additional support and correct foot mechanics.
Night Splints and Braces
- Night Splints: Wearing a splint at night can keep the plantar fascia stretched, reducing morning pain.
- Braces: Daytime braces can provide additional support during activities.
 Advanced Treatments
Advanced Treatments
- Corticosteroid Injections: Injections of corticosteroids can provide temporary relief from severe pain and inflammation.
- Extracorporeal Shock Wave Therapy (ESWT): This non-invasive treatment uses sound waves to stimulate healing in the plantar fascia.
- Platelet-Rich Plasma (PRP) Therapy: PRP involves injecting concentrated platelets from your blood into the affected area to promote healing.
- Plantar Fascia Release Surgery: In severe cases, surgery may be necessary. This procedure involves cutting part of the plantar fascia to release tension and relieve pain.
- Recovery: Post-surgery, a structured recovery plan involving rest, physical therapy, and gradual return to activity is essential for optimal healing.
Exploring these treatment options with a healthcare professional can help you find the most effective approach to managing plantar fasciitis, alleviating pain, and improving your quality of life.

 Advanced Treatments
Advanced Treatments In conclusion, understanding and effectively treating plantar fasciitis is crucial for alleviating pain and improving quality of life. By exploring various treatment options, from home remedies to advanced medical interventions, you can find the best approach to managing this common foot condition. Surgery is typically a last resort, but it can provide significant relief for those who have not found success with other treatments.
In conclusion, understanding and effectively treating plantar fasciitis is crucial for alleviating pain and improving quality of life. By exploring various treatment options, from home remedies to advanced medical interventions, you can find the best approach to managing this common foot condition. Surgery is typically a last resort, but it can provide significant relief for those who have not found success with other treatments.