Table of Contents
Introduction
Charcot foot, a condition that often afflicts individuals with diabetes, is a source of great concern in the medical community. It’s a debilitating disease that can lead to deformity, disability, and even amputation if not appropriately treated. Understanding Charcot foot — its causes, symptoms, treatment options, and prevention strategies — can be vital for those at risk and their caregivers.
So, what exactly is Charcot foot? How is it linked to diabetes? What are the early signs that one should look out for? And perhaps most importantly, how can we prevent and treat this condition? This guide seeks to provide comprehensive answers to these questions and more. Drawing upon expert insights, current research, and practical advice, we offer a deep dive into the complex world of Charcot foot. Whether you’re a patient, a caregiver, or a healthcare provider, you’ll find value and solutions in this detailed exploration. Let’s journey together into understanding this health challenge, demystifying its complexities, and illuminating pathways to effective management.
Stay tuned as we delve into the intricacies of Charcot foot, from its symptoms and causes to the latest treatment strategies and prevention measures. We aim to equip you with the knowledge you need to tackle this condition effectively and improve the quality of life for those affected. Let’s get started.
What is Charcot Foot?
 Charcot foot is a serious condition that affects the bones, joints, and soft tissues of the foot or ankle. Named after the French neurologist Jean-Martin Charcot who first identified it in the 19th century, this disorder is most commonly seen in individuals with peripheral neuropathy, especially those with diabetes.
Charcot foot is a serious condition that affects the bones, joints, and soft tissues of the foot or ankle. Named after the French neurologist Jean-Martin Charcot who first identified it in the 19th century, this disorder is most commonly seen in individuals with peripheral neuropathy, especially those with diabetes.
Definition
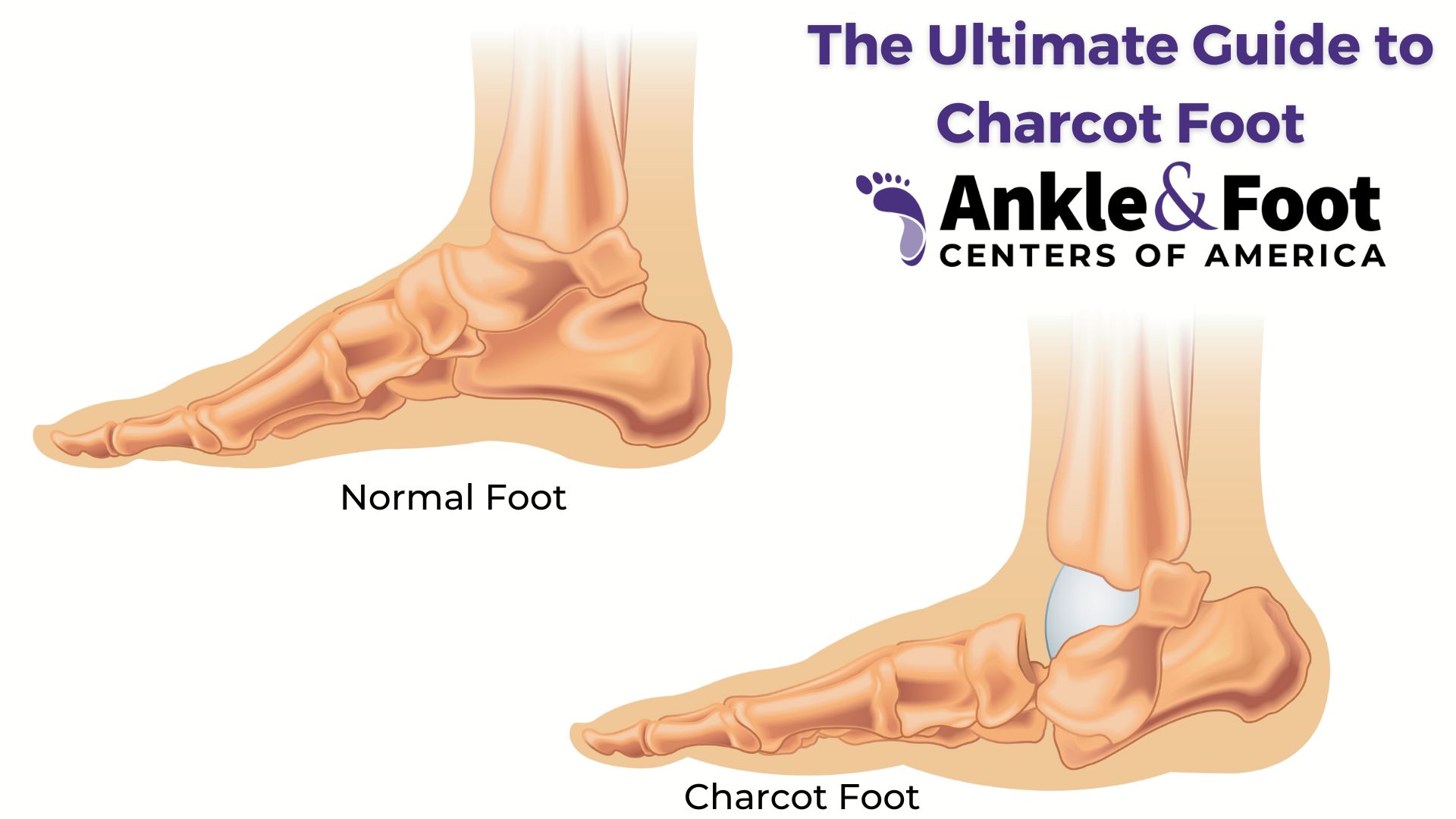
Charcot foot, also known as neurogenic arthropathy, is characterized by the weakening of the bones in the foot that can occur in people who have significant nerve damage (neuropathy). The bones are weakened enough to fracture, and with continued walking, the foot eventually changes shape. Due to numbness in the feet, the fractures often go unnoticed and untreated, leading to a cycle of injury and healing. Over time, the untreated injuries lead to deformity, disability, and in severe cases, amputation.
Brief History
Jean-Martin Charcot first identified this condition during the late 1800s when studying patients with syphilis, a disease which often led to neuropathy. Although the underlying causes of Charcot foot have diversified over the years, the common thread remains: neuropathy is a significant risk factor. Today, diabetes is the most common condition associated with Charcot foot due to the nerve damage that often accompanies uncontrolled blood sugar levels.
Prevalence
Charcot foot is not a common condition, but it is prevalent among certain groups. People with diabetes are particularly at risk, especially those with long-standing or poorly controlled disease. This is due to the fact that high blood sugar levels over time can cause nerve damage, leading to loss of sensation in the feet — a condition known as diabetic neuropathy. According to medical studies, about 0.1% to 0.9% of people with diabetes develop Charcot foot. This figure may seem small, but given the global prevalence of diabetes, the absolute number of individuals affected is significant.
In the next section, we will delve deeper into the symptoms of Charcot foot, helping you understand what to look out for if you or a loved one have been diagnosed with or are at risk of diabetes. Understanding these signs is the first step towards timely treatment and prevention of further complications.
Symptoms of Charcot Foot
Charcot foot can be challenging to diagnose due to its range of symptoms, which can mimic other conditions. However, early detection is essential to prevent severe damage and complications. Therefore, understanding the signs and symptoms of Charcot foot is crucial.
Early Stage Symptoms
In its early stages, symptoms of Charcot foot may be subtle and easily confused with other conditions like sprains or infections. Here are some early warning signs:
warning signs:
- Swelling: One of the first noticeable signs of Charcot foot is swelling, usually without an obvious cause or injury. The swelling typically occurs in the foot or ankle.
- Redness: The affected foot may also appear red or warm to touch. This is due to inflammation and increased blood flow to the area.
- Pain or soreness: Although neuropathy often results in loss of sensation, some people with Charcot foot may experience pain or soreness, especially in the early stages of the condition.
Later Stage Symptoms
As Charcot foot progresses, the symptoms become more distinct. These are primarily due to the weakening and gradual deformation of the foot structure:
- Deformed foot shape: As the bones weaken and fractures occur, the shape of the foot can change. It may develop a noticeable arch or become flat. In severe cases, the foot may appear dislocated.
- Limited mobility: As the foot changes shape, it can become increasingly difficult to walk or move the foot.
- Ulcers or sores: In the later stages, the abnormal foot shape can lead to pressure sores or diabetic foot ulcers, particularly if the person continues to walk on the affected foot.
Knowing these symptoms, especially the early ones, is vital for people at risk of Charcot foot. The earlier the condition is detected, the better the chances are for successful treatment and prevention of serious complications.
In the next section, we will explore the causes and risk factors of Charcot foot, helping you understand why this condition develops and who is most at risk. This knowledge can guide prevention efforts and inform treatment strategies.
Causes and Risk Factors of Charcot Foot
Understanding the causes and risk factors of Charcot foot is crucial in its prevention and management. While the exact cause of Charcot foot is still a subject of study, it’s known that a significant risk factor is peripheral neuropathy, a condition that causes loss of sensation in the affected areas.
Connection with Diabetes
Diabetes is the most common condition associated with Charcot foot.  Long-standing or poorly controlled diabetes can lead to peripheral neuropathy, a condition where the nerves in the feet are damaged, causing loss of sensation. This lack of sensitivity means that a person may not notice small injuries or stresses to the foot, allowing damage to occur without appropriate treatment or rest.
Long-standing or poorly controlled diabetes can lead to peripheral neuropathy, a condition where the nerves in the feet are damaged, causing loss of sensation. This lack of sensitivity means that a person may not notice small injuries or stresses to the foot, allowing damage to occur without appropriate treatment or rest.
In people with diabetes and neuropathy, the bones in the foot can become weakened due to poor blood circulation and high blood glucose levels. This weakening, combined with continued stress on the foot from normal activities like walking, can lead to fractures and dislocations. As these injuries go unnoticed and untreated, the foot structure can change, leading to Charcot foot.
Other Risk Factors
While diabetes is a significant risk factor, other conditions that can lead to peripheral neuropathy also increase the risk of Charcot foot. These include:
- Chronic alcoholism: Long-term excessive consumption of alcohol can damage peripheral nerves, leading to neuropathy.
- Spinal cord injuries and disorders: Conditions that affect the spinal cord can cause neuropathy, including spinal cord injury, disc herniation, and spinal stenosis.
- Certain infections: Some infections, including HIV and leprosy, can cause peripheral neuropathy.
- Hereditary neuropathic conditions: Some inherited conditions, such as Charcot-Marie-Tooth disease, can cause neuropathy and increase the risk of Charcot foot.
In addition to these risk factors, some studies suggest that traumatic injury to the foot or ankle, kidney dialysis, and the use of certain medications like corticosteroids may also increase the risk of Charcot foot.
Recognizing these risk factors is crucial in preventing and managing Charcot foot, particularly in individuals with diabetes. In the next section, we will delve into the process of diagnosing Charcot foot and understanding its stages, a critical aspect of managing this condition effectively.
Diagnosing Charcot Foot
Diagnosing Charcot foot in its early stages is crucial to prevent further damage and complications. Due to its overlapping symptoms with other conditions, such as cellulitis and deep vein thrombosis, Charcot foot can often be challenging to diagnose. However, a combination of clinical examination and imaging tests can help healthcare professionals make an accurate diagnosis.
Stages of Charcot Foot
The progression of Charcot foot is generally divided into three stages:
- Stage I (Development): This is the acute stage, characterized by significant inflammation, redness, and swelling. The foot is often warm to the touch. On an X-ray, one might see signs of bone and joint dislocation or fractures.
- Stage II (Coalescence): This is the phase where the acute symptoms start to subside. Swelling and warmth may decrease, and the broken bones begin to solidify in their abnormal positions.
- Stage III (Reconstruction): In this final stage, the swelling and inflammation are usually resolved, but the foot has now taken on its new, deformed shape.
Diagnostic Tests
Doctors often start with a physical examination, looking out for signs such as swelling, redness, changes in foot shape, and skin ulcers. They’ll also take into account the patient’s medical history, particularly factors like diabetes and neuropathy.
For further confirmation, imaging tests are used:
- X-rays: They are typically the first-line imaging test to look for changes in the bones and joints of the foot. In the early stages, an X-ray may appear normal, even when Charcot foot is present. However, as the condition progresses, X-rays can show fractures and dislocations, as well as changes in the foot’s structure.
- MRI (Magnetic Resonance Imaging): An MRI can detect Charcot foot in its earlier stages better than an X-ray. It can show soft tissue inflammation and bone marrow edema, which are early signs of Charcot foot.
- CT (Computed Tomography) scan: This test can provide detailed images of the bones and can be used to assess the severity of the deformities and plan for any potential surgery.
A timely and accurate diagnosis of Charcot foot is crucial in preventing further progression and deformity. With proper treatment, it’s possible to manage the symptoms and improve the quality of life for individuals affected by this condition. In the upcoming section, we’ll explore the different treatment options available for Charcot foot.
Treatment of Charcot Foot
The treatment of Charcot foot centers on preventing further damage and reducing the risk of complications. Early detection plays a pivotal role in the treatment outcome. When Charcot foot is caught in its early stages, the goal is to halt the progression of the disease. In advanced cases, treatment focuses on managing the symptoms and correcting the foot deformity to improve mobility.
Non-Surgical Treatment
The first line of treatment for Charcot foot is typically non-surgical. The goal is to immobilize the foot to allow the damaged bones to heal and prevent further injury. Non-surgical treatments include:
- Immobilization: The patient is advised to avoid weight-bearing activities to prevent further damage. This is usually accomplished through the use of a cast, brace, or a special boot. Crutches, wheelchairs, or other mobility aids may also be used.
- Custom Shoes and Bracing: Once the initial swelling has decreased and the foot has begun to heal, custom shoes or insoles may be used to distribute weight evenly and prevent ulcers. A brace can provide additional support and prevent further injury.
- Monitoring and Regular Checkups: Regular follow-ups are essential to monitor the healing process, assess the effectiveness of the treatment, and make necessary adjustments. Checkups typically include physical examination and imaging tests.
Surgical Treatment
In some cases, if the deformity is severe or if non-surgical treatments are ineffective, surgery may be considered. The aim is to correct the foot deformity, improve functionality, and prevent further complications. Surgical procedures can include:

- Osteotomy: This involves cutting and realigning the bones to correct the deformity.
- Arthrodesis: In this procedure, the surgeon fuses the bones in the deformed joint to provide stability.
- Ostectomy: This procedure involves removing bony protrusions that could potentially cause ulcers.
- Amputation: In severe cases, when other treatments have failed to control the symptoms, amputation of the affected part may be necessary.
Managing Underlying Conditions
Given that Charcot foot is often linked to underlying conditions like diabetes, managing these conditions is a crucial part of treatment. For diabetics, this includes maintaining blood glucose levels, taking prescribed medications, and regular checkups.
The treatment of Charcot foot is typically long-term and requires significant lifestyle adjustments. In the next section, we will discuss prevention strategies and how to live with Charcot foot, helping those affected to maintain a good quality of life.

Living With and Preventing Charcot Foot
Living with Charcot foot can be challenging, but with the right measures, one can maintain an active life while managing the condition effectively. Likewise, understanding prevention strategies is key to reducing the risk of Charcot foot, especially for high-risk individuals.
Living With Charcot Foot
For those living with Diabetic Charcot foot, adhering to treatment plans and making specific lifestyle adjustments can aid in managing the condition. Here are some key considerations:
- Foot Care: Daily foot inspection is essential to identify any changes or injuries early. This can include signs of ulcers, infection, or changes in foot shape. Any concerns should be reported to a healthcare professional promptly.
- Proper Footwear: Custom shoes or insoles designed to distribute weight evenly across the foot can reduce the risk of ulcers. They can also accommodate any changes in foot shape.
- Activity Modification: Some activities may need to be adjusted to reduce the stress on the foot. Non-weight-bearing activities, such as swimming or cycling, can be good alternatives to walking or running.
- Regular Check-ups: Regular appointments with healthcare professionals help monitor the progression of the condition and make necessary treatment adjustments.
Preventing Strategies
Preventing Charcot foot largely involves managing risk factors, especially peripheral neuropathy. Some key preventive measures include:
- Manage Underlying Conditions: Effective management of conditions like diabetes can reduce the risk of peripheral neuropathy and, consequently, Charcot foot.
- Regular Foot Exams: Regular foot examinations, either self-conducted or by a healthcare professional, can help detect early signs of Charcot foot.
- Prompt Treatment of Foot Injuries: Treating even minor foot injuries promptly can prevent complications that may lead to Charcot foot.
- Healthy Lifestyle: Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding factors like excessive alcohol, can help improve overall foot health.
Living with and preventing Charcot foot involves a holistic approach that focuses on both medical treatments and lifestyle adaptations. With the right strategies, it’s possible to manage this condition effectively and maintain a high quality of life. The next section will provide references to some valuable resources that offer additional information on Charcot foot.
Conclusion
Charcot foot is a serious and complex condition that often results from peripheral neuropathy, particularly in people with diabetes. It is characterized by weakening of the bones in the foot, leading to fractures, dislocations, and ultimately deformities. Despite its severe nature, understanding the signs and symptoms, getting timely diagnosis and appropriate treatment can help manage the condition and prevent further complications.
Non-surgical treatments such as immobilization and custom footwear play a significant role in managing Charcot foot. However, in severe cases, surgical options might be necessary. Above all, successful treatment and management hinge on managing underlying conditions like diabetes and implementing preventive measures such as regular foot exams and prompt treatment of foot injuries.
Living with Charcot foot involves substantial lifestyle modifications and adherence to the treatment plan, but with the right approach and support, individuals can lead an active and fulfilling life.
Remember, while the information in this article is designed to provide you with a better understanding of Charcot foot, it is not a substitute for professional medical advice. Always consult with a healthcare professional for diagnosis and treatment.