Table of Contents
Introduction
Peroneal Tendonitis is a medical condition that affects a significant number of people, particularly athletes and those who engage in high-impact activities. This condition, characterized by the inflammation and degeneration of the peroneal tendons, can cause considerable discomfort and hinder daily activities, making it a critical health issue that requires attention and understanding.
The peroneal tendons are two fibrous cords that run along the outer part of the ankle and the side of the foot. These tendons play a crucial role in foot and ankle movement, helping to stabilize the foot and prevent sprains. When these tendons become inflamed or degenerate due to overuse or injury, it results in a condition known as Peroneal Tendonitis.
Understanding Peroneal Tendonitis is not just essential for those who have been diagnosed with the condition, but also for individuals who engage in activities that put them at risk. By being aware of the causes, symptoms, and treatment options for Peroneal Tendonitis, individuals can take proactive steps to prevent the onset of this condition or manage it effectively if they have already been diagnosed.
In this comprehensive guide, we will delve into the intricacies of Peroneal Tendonitis, exploring its causes, symptoms, diagnosis process, treatment options, and prevention strategies. We will also answer frequently asked questions about this condition and provide additional information related to it. Whether you are a patient, a healthcare professional, an athlete, or simply an individual seeking to broaden your knowledge about this health issue, this guide aims to provide you with a thorough understanding of Peroneal Tendonitis.
Understanding Peroneal Tendonitis
Peroneal Tendonitis is a condition that primarily affects the two peroneal tendons in the foot. These tendons, known as the peroneus longus and the peroneus brevis, run side by side behind the outer ankle bone. The peroneus longus extends under the foot and attaches near the inside of the arch, while the peroneus brevis attaches to the outside of the foot. These tendons play a crucial role in stabilizing the foot and ankle and protecting them from sprains.
What is Peroneal Tendonitis?
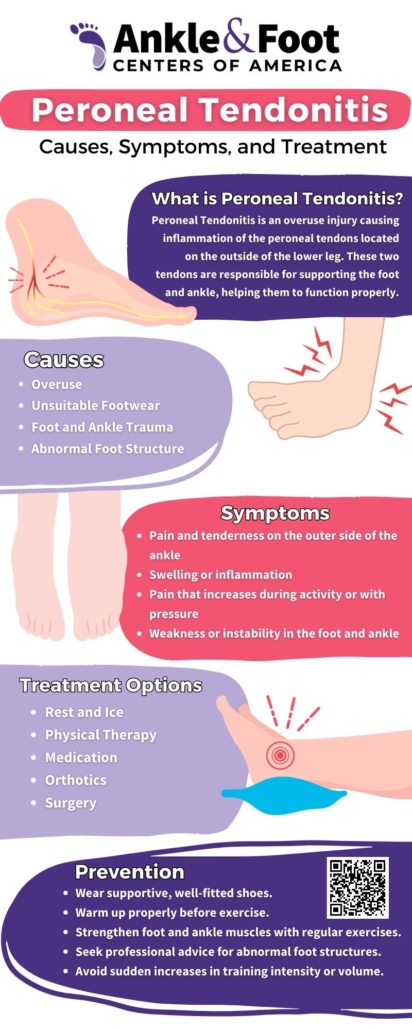
 Peroneal Tendonitis is characterized by the inflammation and degeneration of the peroneal tendons. This condition typically arises when the tendons are subjected to repetitive tension or stress over time, leading to micro-tears. The body responds to these micro-tears with inflammation, which is intended to heal the area. However, if the stress continues and the body doesn’t get a chance to complete the healing process, the inflammation and damage persist, leading to tendonitis.
Peroneal Tendonitis is characterized by the inflammation and degeneration of the peroneal tendons. This condition typically arises when the tendons are subjected to repetitive tension or stress over time, leading to micro-tears. The body responds to these micro-tears with inflammation, which is intended to heal the area. However, if the stress continues and the body doesn’t get a chance to complete the healing process, the inflammation and damage persist, leading to tendonitis.
In Peroneal Tendonitis, patients often experience pain along the outside of the foot or behind the ankle, particularly during activity. This pain can make it difficult to walk or participate in activities, particularly those that involve repetitive ankle motion or put stress on the tendons.
Causes of Peroneal Tendonitis
Peroneal Tendonitis can be caused by a variety of factors. One of the most common causes is overuse, particularly in activities that involve repetitive ankle motion. This includes running, dancing, or other sports that put a lot of stress on the peroneal tendons. Over time, this repetitive stress can lead to inflammation and degeneration of the tendons.
Sudden injuries can also lead to Peroneal Tendonitis. This includes acute ankle sprains, where the rapid and forceful stretching of the peroneal tendons can cause micro-tears and subsequent inflammation.
Another common cause is an increased load and friction between the tendon and bone. This can occur due to structural abnormalities in the foot, such as high arches or a hindfoot varus position, where the heel turns inward. These abnormalities can cause the peroneal tendons to rub against the bone, leading to irritation and inflammation.
Other factors that can contribute to the development of Peroneal Tendonitis include a sudden increase in training intensity or duration, improper training techniques, and inadequate footwear. Certain conditions can also increase the risk of developing Peroneal Tendonitis, including diabetes, osteoarthritis, rheumatoid arthritis, gout, and other conditions that can cause systemic inflammation.
Understanding these causes is crucial for the prevention and management of Peroneal Tendonitis. By identifying and addressing these risk factors, individuals can reduce their risk of developing this condition and ensure that they are taking the appropriate steps to protect their peroneal tendons.
Recognizing the Symptoms of Peroneal Tendonitis
Recognizing the symptoms of Peroneal Tendonitis is the first step towards getting appropriate treatment. The symptoms can vary in intensity and duration, depending on the severity of the condition and the individual’s activity level. However, there are common signs and symptoms that individuals can look out for.
Common Symptoms
The most common symptom of Peroneal Tendonitis is pain at the back and outside of the foot and ankle. This pain is typically associated with activity, such as walking or running, and tends to lessen with rest. The pain may be sharp or aching in nature and can range from mild to severe. It’s important to note that the pain associated with Peroneal Tendonitis is usually localized to the area around the peroneal tendons, and does not typically spread to other areas of the foot or leg.
In addition to pain, individuals with Peroneal Tendonitis may also experience swelling in the area of the peroneal tendons. This swelling can make the back and outside of the ankle appear puffy or enlarged. The area may also feel warm to the touch, which is a sign of inflammation.
How Symptoms Change with Activity
As mentioned earlier, the symptoms of Peroneal Tendonitis often worsen with activity and lessen with rest. This is because activity, particularly activities that involve repetitive ankle motion, can put stress on the inflamed and degenerated tendons, leading to increased pain and swelling. On the other hand, rest can allow the inflammation to subside and the tendons to heal, leading to a reduction in symptoms.
However, it’s important to note that while rest can help alleviate the symptoms of Peroneal Tendonitis, it does not address the underlying cause of the condition. Therefore, individuals with Peroneal Tendonitis should seek medical attention to get a proper diagnosis and treatment plan, rather than simply resting and hoping the condition will resolve on its own.
Physical Signs of Peroneal Tendonitis
In addition to pain and swelling, there are several physical signs that can indicate Peroneal Tendonitis. One of these signs is thickened tendons. The peroneal tendons may feel thicker or harder than normal, and this can sometimes be felt through the skin at the back and outside of the ankle.
Another physical sign is pain with inversion, which is when the sole of the foot is turned inwards. This movement stretches the peroneal tendons and can cause pain in individuals with Peroneal Tendonitis.
Finally, some individuals with Peroneal Tendonitis may experience instability of the ankle when bearing weight. This can make it difficult to stand or walk, particularly on uneven surfaces.
Recognizing these symptoms and seeking medical attention can help ensure that Peroneal Tendonitis is diagnosed and treated promptly, reducing the risk of complications and promoting a quicker recovery.
Diagnosis of Peroneal Tendonitis
Diagnosing Peroneal Tendonitis involves a series of steps that allow healthcare professionals to accurately identify the condition and rule out other potential causes of the symptoms. The process typically involves a discussion of the patient’s medical history, a physical examination, a review of symptoms, and imaging tests.
The Diagnosis Process
The first step in diagnosing Peroneal Tendonitis is usually a discussion of the patient’s medical history. The healthcare provider will ask about the patient’s symptoms, including when they started, what activities exacerbate or alleviate them, and whether the patient has experienced any recent injuries that could have caused them. The provider will also ask about the patient’s lifestyle, including their physical activity level and the type of footwear they typically wear. This information can help the provider determine whether the patient’s symptoms are consistent with Peroneal Tendonitis and whether there are any risk factors that could have contributed to the condition.
Next, your foot and ankle specialist will perform a physical examination. This typically involves palpating (feeling) the area around the peroneal tendons to check for swelling, warmth, or thickening. The provider may also ask the patient to perform certain movements, such as inverting the foot or standing on tiptoe, to see if these movements cause pain. In some cases, an expert podiatrist may also perform a manual resistance test, where they apply pressure to the foot or ankle while the patient tries to move it. This can help the provider assess the strength and function of the peroneal tendons.
In addition to the medical history and physical exam, the healthcare provider will also review the patient’s symptoms in detail. They will ask about the nature of the pain (e.g., is it sharp or aching?), its location (e.g., is it localized to the back and outside of the ankle, or does it spread to other areas?), and its timing (e.g., does it worsen with activity and improve with rest?). This information can help the provider differentiate Peroneal Tendonitis from other conditions that can cause similar symptoms, such as a sprained ankle or a stress fracture.
Finally, if the foot doctor suspects Peroneal Tendonitis based on the medical history, physical exam, and symptom review, they may order imaging tests to confirm the diagnosis. These tests can include an X-ray, which can rule out bone abnormalities or fractures; an MRI (Magnetic Resonance Imaging), which can provide detailed images of the soft tissues and can show inflammation or degeneration in the peroneal tendons; a CT (Computed Tomography) scan, which can provide cross-sectional images of the foot and ankle and can show any bone abnormalities that could be causing the symptoms; or an ultrasound, which can provide real-time images of the tendons and can show whether they are moving normally.
The diagnosis of Peroneal Tendonitis is a thorough process that allows healthcare providers to accurately identify the condition and develop an appropriate treatment plan. If you are experiencing symptoms that you suspect may be due to Peroneal Tendonitis, it’s important to seek medical attention to get a proper diagnosis and start treatment as soon as possible.

Treatment Options for Peroneal Tendonitis
Once Peroneal Tendonitis has been diagnosed, the next step is to develop a treatment plan that addresses the underlying cause of the condition, alleviates the symptoms, and promotes healing of the peroneal tendons. Treatment options for Peroneal Tendonitis can be broadly divided into non-surgical treatments and surgical treatments.
Non-Surgical Treatments
 Non-surgical treatments are typically the first line of treatment for Peroneal Tendonitis. These treatments aim to reduce inflammation, alleviate pain, and promote healing of the peroneal tendons. They can also help to prevent further damage to the tendons and reduce the risk of complications.
Non-surgical treatments are typically the first line of treatment for Peroneal Tendonitis. These treatments aim to reduce inflammation, alleviate pain, and promote healing of the peroneal tendons. They can also help to prevent further damage to the tendons and reduce the risk of complications.
One of the most common non-surgical treatments for Peroneal Tendonitis is the RICE protocol, which stands for Rest, Ice, Compression, and Elevation. Rest involves reducing or avoiding activities that exacerbate the symptoms, to give the tendons a chance to heal. Ice can be applied to the area to reduce inflammation and numb the pain. Compression, such as wearing an elastic bandage or a Peroneal Tendonitis brace, can help to reduce swelling and provide support to the area. Elevation involves raising the foot above the level of the heart, to help reduce swelling.
Medication can also be used to manage the symptoms of Peroneal Tendonitis. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help to reduce inflammation and alleviate pain. In some cases, a healthcare provider may also recommend steroid injections, which can provide more targeted and potent anti-inflammatory effects.
Physical therapy is another important component of non-surgical treatment for the condition. A physical therapist can provide Peroneal Tendonitis exercises to strengthen the muscles around the ankle, improve flexibility, and promote healing of the tendons. They can also provide advice on proper footwear and modifications to training or activity levels, to prevent further damage to the tendons.
Other non-surgical treatments for Peroneal Tendonitis can include bracing, to provide support to the ankle and reduce strain on the tendons; orthotics, to correct any structural abnormalities in the foot that could be contributing to the condition; and changes in training structure or technique, to reduce stress on the tendons.
Surgical Treatments
Surgical treatments for Peroneal Tendonitis are typically considered only if non-surgical treatments have not been effective, or if the condition is severe. The goal of surgery is to repair the damaged tendons and address any underlying issues that could be contributing to the condition.
There are several types of surgery that can be used to treat Peroneal Tendonitis. One of these is a tendon release, which involves cutting the tendon to relieve tension and allow it to heal. Another is a tendon repair, which involves stitching the torn tendon back together.
The type of surgery required will depend on the severity of the condition, the patient’s overall health, and their personal preferences and goals. The healthcare provider will discuss the options with the patient and help them make an informed decision.
Regardless of the type of treatment chosen, it’s important to remember that recovery from Peroneal Tendonitis takes time and patience. It’s crucial to follow the healthcare provider’s instructions and to continue with treatment even after the symptoms have improved, to ensure a full and lasting recovery.
Preventing Peroneal Tendonitis
Preventing Peroneal Tendonitis is crucial, especially for individuals who are at a higher risk due to their lifestyle or physical activities. Prevention strategies aim to reduce the strain on the peroneal tendons, correct any underlying biomechanical issues, and promote overall foot and ankle health.
Prevention Strategies
 One of the most effective strategies for preventing Peroneal Tendonitis is wearing appropriate footwear. Shoes should provide good arch support, cushioning, and stability to reduce strain on the peroneal tendons. For individuals who participate in sports or physical activities, sport-specific shoes may be beneficial. For example, running shoes are designed to absorb the impact of each step, reducing the load on the tendons.
One of the most effective strategies for preventing Peroneal Tendonitis is wearing appropriate footwear. Shoes should provide good arch support, cushioning, and stability to reduce strain on the peroneal tendons. For individuals who participate in sports or physical activities, sport-specific shoes may be beneficial. For example, running shoes are designed to absorb the impact of each step, reducing the load on the tendons.
Stretching the calf and peroneal muscles is another important prevention strategy. Tight muscles can increase the strain on the tendons, so regular stretching can help to maintain flexibility and reduce the risk of the condition. A physical therapist can provide guidance on appropriate stretching and Peroneal Tendonitis exercises.
Gradually increasing training workload can also help to prevent Peroneal Tendonitis. A sudden increase in activity level or intensity can put excessive strain on the tendons, leading to inflammation and degeneration. Therefore, individuals should aim to increase their activity level gradually, giving the tendons time to adapt to the increased load.
Maintaining a healthy body weight can also help to prevent Peroneal Tendonitis. Excess weight can put additional strain on the tendons, increasing the risk of inflammation and degeneration. Therefore, maintaining a healthy body weight through a balanced diet and regular physical activity can help to reduce the load on the tendons.
Using ankle braces or supportive shoes can provide additional support to the foot and ankle, reducing strain on the peroneal tendons. This can be particularly beneficial for individuals who have structural abnormalities in the foot, such as high arches, that increase their risk of Peroneal Tendonitis.
Finally, maintaining a level of activity throughout recovery from Peroneal Tendonitis can help to prevent the condition from recurring. Complete rest can lead to muscle weakness and stiffness, which can increase the risk of re-injury once activity is resumed. Therefore, individuals should aim to maintain a level of activity that does not exacerbate their symptoms, and gradually increase their activity level as their condition improves.
Preventing Peroneal Tendonitis requires a proactive approach to foot and ankle health. By implementing these strategies, individuals can reduce their risk of this condition and promote overall foot and ankle health.
Prognosis and Recovery from Peroneal Tendonitis
The prognosis and recovery from Peroneal Tendonitis largely depend on the severity of the condition, the effectiveness of the treatment, and the individual’s adherence to the treatment plan. With appropriate treatment and care, most individuals can expect to make a full recovery.
Recovery Time
The recovery time from Peroneal Tendonitis can vary significantly from one individual to another. For some, symptoms may resolve within a few weeks of starting treatment, while others may require several months to fully recover. This variability is largely due to differences in the severity of the condition, the effectiveness of the treatment, and the individual’s overall health and healing capacity.
During the recovery period, it’s crucial to adhere to the treatment plan and to avoid activities that exacerbate the symptoms. This typically involves rest, physical therapy exercises, medication, and possibly the use of braces or orthotics. Over time, as the inflammation subsides and the tendons heal, individuals can gradually resume their normal activities.
Prognosis
The prognosis for the condition is generally good, with most individuals achieving a full recovery with appropriate Peroneal Tendonitis treatment. However, it’s important to note that recovery requires time and patience. The peroneal tendons, like all tendons in the body, have a relatively poor blood supply, which can slow the healing process. Therefore, it’s crucial to give the body the time it needs to heal and to avoid rushing the recovery process.
Once recovered, most individuals can return to their previous level of activity without any lasting effects. However, it’s important to continue with preventive measures, such as wearing appropriate footwear and maintaining flexibility and strength in the foot and ankle, to reduce the risk of recurrence.
Importance of Treatment
 Untreated Peroneal Tendonitis can lead to a number of complications, making treatment essential. One potential complication is a tear in the peroneal tendons, which can occur if the inflammation and degeneration are allowed to progress. This can lead to significant pain and disability, and may require surgical repair.
Untreated Peroneal Tendonitis can lead to a number of complications, making treatment essential. One potential complication is a tear in the peroneal tendons, which can occur if the inflammation and degeneration are allowed to progress. This can lead to significant pain and disability, and may require surgical repair.
Another potential complication is chronic instability of the ankle. The peroneal tendons play a crucial role in stabilizing the foot and ankle, so damage to these tendons can lead to recurrent ankle sprains and a feeling of instability when walking or standing.
Finally, untreated Peroneal Tendonitis can lead to nerve damage. The peroneal nerve runs close to the peroneal tendons, and prolonged inflammation in this area can potentially affect the nerve, leading to symptoms such as numbness, tingling, or weakness in the foot and ankle.
Therefore, if you suspect that you have Peroneal Tendonitis, it’s crucial to seek medical attention to get a proper diagnosis and treatment. This can help to alleviate your symptoms, promote healing, and reduce the risk of complications.
FAQs about Peroneal Tendonitis
In this section, we will address some of the most frequently asked questions about Peroneal Tendonitis. These questions cover a range of topics, from the basics of what the condition is, to more detailed inquiries about its treatment and prevention.
What is Peroneal Tendonitis?
Peroneal Tendonitis is a condition characterized by inflammation and degeneration of the peroneal tendons, which are located along the outer ankle bone and side of the foot. This condition typically results from overuse or sudden injury, leading to pain and difficulty in movement.
How is Peroneal Tendonitis treated?
Treatment for Peroneal Tendonitis typically involves a combination of rest, medication, physical therapy, and in some cases, surgery. The goal of treatment is to reduce inflammation, alleviate pain, and promote healing of the tendons. It’s important to follow the treatment plan closely and to continue with preventive measures even after the symptoms have improved.
What causes Peroneal Tendonitis?
Peroneal Tendonitis is often caused by overuse, sudden injury, or increased load and friction between the tendon and bone. Other factors, such as improper training techniques, inadequate footwear, and certain conditions like diabetes, osteoarthritis, and rheumatoid arthritis, can also contribute to the development of this condition.
How long does it take for Peroneal Tendonitis to heal?
The healing time for Peroneal Tendonitis can vary from a few weeks to a few months, depending on the severity of the condition and the individual’s adherence to the treatment plan. It’s crucial to give the body the time it needs to heal and to avoid rushing the recovery process.
What are the symptoms of Peroneal Tendonitis?
The most common symptoms of Peroneal Tendonitis include pain at the back and outside of the foot and ankle, swelling, redness, warmth around the tendon, thickened tendons, pain with inversion, and instability of the ankle when bearing weight.
Can Peroneal Tendonitis lead to other complications?
If left untreated, Peroneal Tendonitis can lead to complications such as a tear in the peroneal tendons, chronic instability of the ankle, and nerve damage. Therefore, it’s crucial to seek medical attention if you suspect you have Peroneal Tendonitis.
What are the preventive measures for Peroneal Tendonitis?
Preventive measures for Peroneal Tendonitis include wearing appropriate footwear, stretching the calf and peroneal muscles, gradually increasing training workload, maintaining a healthy body weight, using ankle braces or supportive shoes, and maintaining a level of activity throughout recovery.
What are the conservative treatments for Peroneal Tendonitis?
Conservative treatments for Peroneal Tendonitis include rest, ice, compression, elevation (RICE), medication (NSAIDs, steroid injections), physical therapy, bracing, orthotics, and changes in training structure or technique.
How effective are orthotics in treating Peroneal Tendonitis?
Orthotics can be very effective in treating Peroneal Tendonitis, especially if the condition is caused by structural abnormalities in the foot. Orthotics can provide support, correct alignment, and reduce strain on the tendons, promoting healing and preventing further damage.
What is the role of physical therapy in treating Peroneal Tendonitis?
Physical therapy plays a crucial role in the treatment of Peroneal Tendonitis. A physical therapist can provide exercises to strengthen the muscles around the ankle, improve flexibility, and promote healing of the tendons. They can also provide advice on proper footwear and modifications to training or activity levels, to prevent further damage to the tendons. Physical therapy is often a key component of a comprehensive treatment plan for Peroneal Tendonitis.
These FAQs provide a comprehensive overview of Peroneal Tendonitis, covering key aspects of the condition, its treatment, and prevention. By understanding these aspects, individuals can better manage the condition and make informed decisions about their health.
Additional Information on Peroneal Tendonitis
Beyond the basic understanding of Peroneal Tendonitis, there are several related topics and queries that can provide a more comprehensive understanding of the condition. These topics delve into the different aspects of Peroneal Tendonitis, including related conditions, management strategies, and the impact of the condition on various activities.
Peroneal Tendon Disorders
Peroneal Tendon Disorders refer to a group of conditions that affect the peroneal tendons. These can include Peroneal Tendonitis, peroneal tendon tears, and peroneal tendon dislocation. Each of these conditions has its own unique set of symptoms, causes, and treatment strategies.
Peroneal Tendinopathy
Peroneal Tendinopathy is a term that is often used interchangeably with Peroneal Tendonitis. However, tendinopathy is a broader term that refers to any disease of a tendon, while tendonitis specifically refers to inflammation of a tendon.
Peroneal Tendonitis Management
Managing Peroneal Tendonitis involves a combination of treatments aimed at reducing inflammation, alleviating pain, and promoting healing of the tendons. This can include rest, medication, physical therapy, and in some cases, surgery.
Peroneal Tendonitis and Physical Therapy
Physical therapy plays a crucial role in the treatment of Peroneal Tendonitis. A physical therapist can provide exercises to strengthen the muscles around the ankle, improve flexibility, and promote healing of the tendons. They can also provide advice on proper footwear and modifications to training or activity levels, to prevent further damage to the tendons.
Peroneal Tendonitis and Walking or Running
Walking or running can exacerbate the symptoms of Peroneal Tendonitis, as these activities put strain on the peroneal tendons. However, with appropriate treatment and modifications to technique or footwear, individuals with Peroneal Tendonitis can often return to these activities without pain.
Peroneal Tendinopathy and Diabetes
Diabetes can increase the risk of developing Peroneal Tendonitis, as high blood sugar levels can lead to damage in the tendons. Therefore, individuals with diabetes should take extra precautions to prevent Peroneal Tendonitis, such as wearing appropriate footwear and maintaining good blood sugar control.
Can My Bunion Return After Surgery?
Although bunion surgery has a high success rate, there is a chance that a bunion could recur. This is more likely if the underlying cause of the bunion, such as faulty foot mechanics or improper footwear, is not addressed. Your surgeon will discuss strategies to reduce the risk of recurrence, including choosing appropriate footwear and possibly using orthotic devices. Regular follow-up appointments after surgery are important to monitor your progress and catch any potential problems early.
Peroneal Tendonitis Symptoms
The symptoms of Peroneal Tendonitis typically include pain at the back and outside of the foot and ankle, swelling, redness, warmth around the tendon, thickened tendons, pain with inversion, and instability of the ankle when bearing weight.
Peroneal Tendon Tear and Peroneal Tendonitis
A tear in the peroneal tendons is a potential complication of untreated Peroneal Tendonitis. This can lead to significant pain and disability, and may require surgical repair.
Acute Injuries of the Peroneal Tendons
Acute injuries of the peroneal tendons, such as a sudden tear or dislocation, can cause symptoms similar to Peroneal Tendonitis. These injuries typically require immediate medical attention and may require surgical treatment.
Peroneal Tendon Injuries
Peroneal Tendon Injuries refer to any injury that affects the peroneal tendons. This can include Peroneal Tendonitis, as well as more acute injuries such as tears or dislocations.
Understanding these related topics can provide a more comprehensive understanding of Peroneal Tendonitis, and can help individuals to better manage the condition and make informed decisions about their health.
Conclusion
Peroneal Tendonitis is a condition that affects the peroneal tendons, causing pain and difficulty in movement. It is often caused by overuse or sudden injury, and can be exacerbated by factors such as improper training techniques, inadequate footwear, and certain underlying conditions.
The diagnosis of Peroneal Tendonitis involves a thorough evaluation of the patient’s medical history, physical examination, review of symptoms, and imaging tests. Once diagnosed, treatment typically involves a combination of rest, medication, physical therapy, and in some cases, surgery. With appropriate treatment, most individuals can expect to make a full recovery.
Preventing the condition is crucial, especially for individuals who are at a higher risk due to their lifestyle or physical activities. Preventive measures include wearing appropriate footwear, stretching the calf and peroneal muscles, gradually increasing training workload, maintaining a healthy body weight, using ankle braces or supportive shoes, and maintaining a level of activity throughout recovery.
While the recovery time from Peroneal Tendonitis can vary, the prognosis is generally good. However, it’s important to remember that recovery requires time and patience, and it’s crucial to follow the healthcare provider’s instructions and to continue with treatment even after the symptoms have improved.
If left untreated, Peroneal Tendonitis can lead to complications such as a tear in the peroneal tendons, chronic instability of the ankle, and nerve damage. Therefore, if you suspect that you have Peroneal Tendonitis, it’s crucial to seek medical attention to get a proper diagnosis and treatment.
In conclusion, Peroneal Tendonitis is a manageable condition with a good prognosis, provided that it is diagnosed early and treated appropriately. By understanding the condition, its causes, symptoms, treatment, and prevention strategies, individuals can take proactive steps to manage Peroneal Tendonitis and maintain their foot and ankle health.