Table of Contents
Introduction
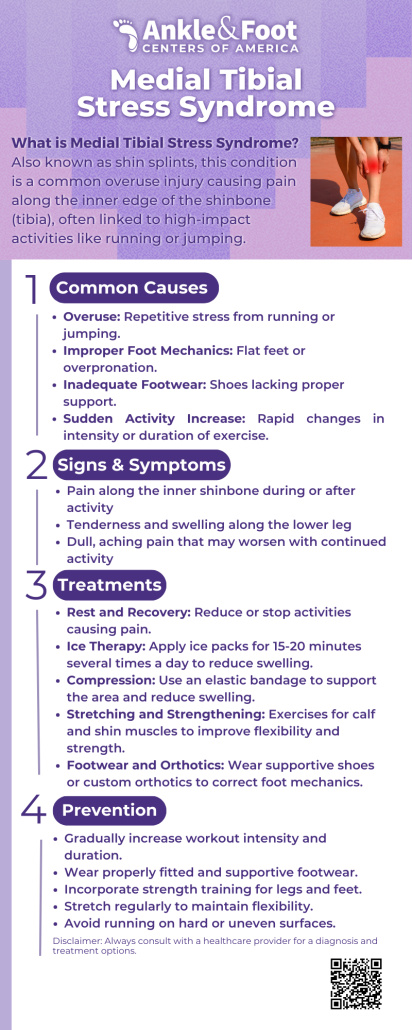
Medial Tibial Stress Syndrome (MTSS), commonly known as shin splints, is a frequent overuse injury causing pain along the inner shinbone. It often affects individuals engaged in high-impact activities, such as running, dancing, or jumping. Consulting a podiatrist can be crucial for accurate diagnosis and effective management.
Recognizing the symptoms and understanding the causes of MTSS are essential steps in finding relief and preventing recurrence. Fortunately, with a combination of tailored treatments and exercises, you can stay active and pain-free while addressing this condition.
What is Medial Tibial Stress Syndrome?
 Medial Tibial Stress Syndrome (MTSS), also called shin splints, is pain along the inner shinbone (tibia). It happens due to repetitive stress on the muscles, tendons, and bones in the lower leg.
Medial Tibial Stress Syndrome (MTSS), also called shin splints, is pain along the inner shinbone (tibia). It happens due to repetitive stress on the muscles, tendons, and bones in the lower leg.
Often, MTSS affects athletes who run or jump frequently. As a result, the repeated activity causes inflammation in the thin tissue surrounding the tibia, eventually leading to discomfort. Furthermore, over time, this pain can worsen if not treated.
Thankfully, understanding what causes medial tibial stress syndrome and recognizing its symptoms can significantly help with early prevention. Moreover, by addressing the issue early, you can avoid more serious problems like stress fractures.
Symptoms of Medial Tibial Stress Syndrome
The symptoms of medial tibial stress syndrome (MTSS) typically develop gradually and worsen with continued activity. Recognizing these signs early is crucial to preventing further complications.
- Pain along the inner shinbone: This is the most common symptom, often described as a dull ache or sharp discomfort.
- Tenderness or swelling: The inner edge of the shin may feel sore or slightly swollen to the touch.
- Worsening pain with activity: Pain tends to increase during high-impact activities like running or jumping and may persist afterward.
- Relief during rest: The discomfort usually subsides when resting but can return once physical activity resumes.
These symptoms can mimic other conditions, such as stress fractures. Therefore, addressing medial tibial stress syndrome symptoms promptly is essential to avoid more severe injuries.
What Causes Medial Tibial Stress Syndrome?
 Understanding what causes medial tibial stress syndrome not only helps in preventing the condition but also ensures that its symptoms are managed effectively. A podiatrist can help identify biomechanical issues and recommend appropriate interventions to reduce tibial stress.
Understanding what causes medial tibial stress syndrome not only helps in preventing the condition but also ensures that its symptoms are managed effectively. A podiatrist can help identify biomechanical issues and recommend appropriate interventions to reduce tibial stress.
- Overtraining or sudden activity increase: Rapidly increasing the intensity or duration of workouts can strain the shinbone and surrounding tissues.
- Improper footwear: Wearing shoes without proper support can lead to uneven stress on the tibia.
- Biomechanical issues: Flat feet, high arches, or poor running mechanics can alter the distribution of forces, increasing strain on the lower leg.
- Hard or uneven surfaces: Exercising on hard or irregular surfaces places extra impact on the shinbone.
- Weak or tight muscles: Insufficient strength or flexibility in the calves, ankles, or feet can contribute to poor shock absorption.
Medial Tibial Stress Syndrome Treatment Options
 Treating Medial Tibial Stress Syndrome (MTSS) involves reducing pain, promoting healing, and preventing recurrence. Below are effective treatment options:
Treating Medial Tibial Stress Syndrome (MTSS) involves reducing pain, promoting healing, and preventing recurrence. Below are effective treatment options:
- Rest and activity modification: Reduce high-impact activities like running or jumping to allow the shinbone and surrounding tissues to recover.
- Ice therapy: Apply ice packs to the affected area for 15–20 minutes several times a day to reduce pain and inflammation.
- Compression and elevation: Wrapping the leg with a compression bandage and keeping it elevated can help reduce swelling.
- Proper footwear: Switch to shoes with good arch support or use custom orthotics to improve alignment and reduce stress on the tibia.
- Stretching and strengthening exercises: Incorporate calf stretches, foot strengthening, and other medial tibial stress syndrome exercises to improve muscle balance and flexibility.
- Cross-training: Engage in low-impact activities like swimming or cycling to maintain fitness without overloading the shins.
- Physical therapy: A physical therapist can provide tailored exercises and techniques to address biomechanical issues.
Severe cases may require more advanced treatments, such as immobilization or shockwave therapy. By addressing medial tibial stress syndrome treatment early, individuals can recover faster and prevent future occurrences.
Medial Tibial Stress Syndrome Exercises for Recovery and Prevention
 Incorporating the right exercises can aid recovery from Medial Tibial Stress Syndrome (MTSS) and reduce the risk of recurrence. These exercises focus on strengthening, stretching, and improving flexibility in the lower leg.
Incorporating the right exercises can aid recovery from Medial Tibial Stress Syndrome (MTSS) and reduce the risk of recurrence. These exercises focus on strengthening, stretching, and improving flexibility in the lower leg.
- Calf Stretches: Stretching the calf muscles helps alleviate tension in the lower leg.
- Stand facing a wall, placing your hands on it for support.
- Step one leg back, keeping the heel flat on the ground and the knee straight.
- Hold for 20–30 seconds, then switch legs.
- Toe Taps: Strengthen the muscles around the shinbone to improve support.
- Sit in a chair with your feet flat on the ground.
- Lift your toes toward the ceiling while keeping your heels on the ground.
- Repeat for 10–15 repetitions.
- Foot Arch Strengthening: Supporting the foot arch can help reduce strain on the tibia.
- While seated, place a towel on the floor and curl your toes to pull it toward you.
- Repeat for 2–3 sets of 10 repetitions per foot.
- Ankle Circles: Increase flexibility and improve blood flow.
- Sit or lie down with one leg extended.
- Rotate the ankle in a circular motion 10 times in each direction.
- Eccentric Calf Raises: Build strength in the calf muscles to better absorb impact.
- Stand on a step or ledge with your heels hanging off the edge.
- Raise up onto your toes, then slowly lower your heels below the step level.
- Perform 2–3 sets of 10–12 repetitions.
- Hip and Core Strengthening: Strong hips and core improve running form and reduce tibial stress.
- Include exercises like clamshells, bridges, and planks in your routine.
By regularly performing these medial tibial stress syndrome exercises, you can enhance recovery and protect against future injuries. Always start slowly and increase intensity as your pain subsides and strength improves.
Preventing Medial Tibial Stress Syndrome
If you’re unsure about the right footwear or experience persistent discomfort, a podiatrist can assess your foot mechanics and provide recommendations for custom orthotics or training modifications.
- Gradual Training Progression: Increase the intensity, duration, or frequency of your workouts gradually. Avoid sudden spikes in activity, as they place undue stress on the tibia.
- Wear Proper Footwear: Use shoes with adequate arch support and cushioning. If needed, consider custom orthotics to address specific biomechanical issues.
- Incorporate Cross-Training: Alternate high-impact activities like running with low-impact options such as swimming or cycling to reduce repetitive stress.
- Strengthen Muscles: Regularly perform exercises that target the calves, shins, and foot arches to build strength and support.
- Stretch Regularly: Stretch your calves, Achilles tendon, and hamstrings to maintain flexibility and prevent tightness that can lead to shin splints.
- Run on Softer Surfaces: Whenever possible, choose softer surfaces, such as trails or grass, to reduce the impact on your legs.
- Pay Attention to Pain: Listen to your body and rest if you experience discomfort. Continuing activity while in pain increases the risk of developing MTSS.
- Maintain Proper Form: Focus on good running technique to evenly distribute forces through the legs and avoid unnecessary strain on the shins.
By implementing these strategies, you can effectively prevent medial tibial stress syndrome and enjoy pain-free physical activity. Taking small, consistent steps now can save you from long-term discomfort later.

Conclusion
Medial Tibial Stress Syndrome (MTSS), or shin splints, is a common yet preventable condition that often affects many athletes and active individuals. By thoroughly understanding its causes, recognizing the symptoms early, and consistently implementing effective treatments and exercises, you can recover faster and significantly prevent it from recurring.
For expert evaluation and treatment options, trust the specialists at Ankle & Foot Centers of America to help you get back on track pain-free. Your journey to healthy, active living starts here!