Diabetic neuropathy, a widespread complication of diabetes, manifests in nerve damage that results from long-term high blood sugar levels. It is a silent epidemic, often developing over the years without immediate symptoms, affecting millions of individuals globally. Its potential impact on life can be debilitating, affecting mobility and leading to severe pain.
At the Ankle & Foot Centers of America, we believe that managing diabetic neuropathy doesn’t have to be a solitary journey. Our team of skilled professionals, including board-certified podiatrist Richard Kaufman, is equipped with the knowledge, understanding, and commitment necessary for providing effective and compassionate care.
This blog post aims to offer a comprehensive understanding of diabetic neuropathy. It serves as a guide to understanding the causes, symptoms, diagnosis, treatment options, and preventative measures of this condition. Furthermore, we’ll delve into a case study that illustrates how our tailored approach to diabetic neuropathy management positively impacts our patients’ lives. Whether you’re a patient suffering from this condition or a medical professional looking to expand your understanding, this guide will provide valuable insights.
Table of Contents
Understanding Diabetic Neuropathy
What is Diabetic Neuropathy?
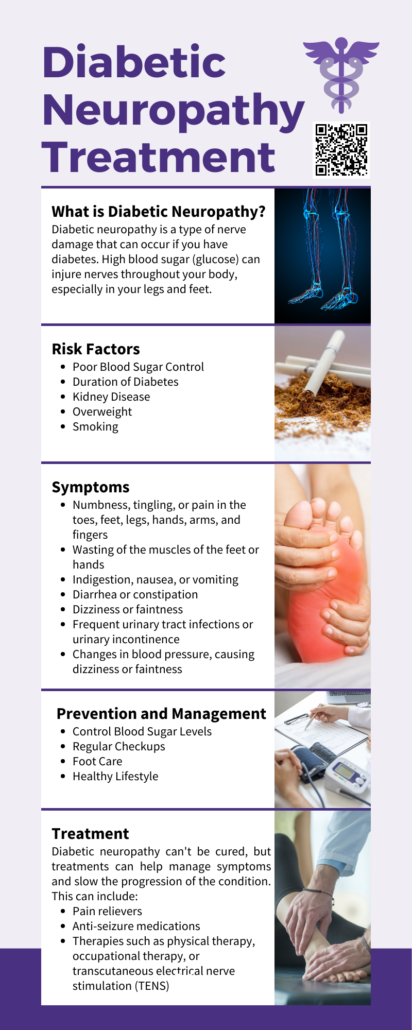
Diabetic neuropathy is a group of nerve disorders caused by prolonged elevated blood glucose levels often seen in individuals with diabetes. While neuropathy can affect various body parts, the extremities, particularly the legs and feet, are usually the first to show symptoms.
The damage associated with diabetic neuropathy can be widespread, affecting the peripheral nerves responsible for sensation, autonomic nerves controlling internal organs, and even motor nerves responsible for muscle movement. The symptoms associated with this condition depend on the type and extent of nerve damage. They can range from numbness or tingling sensations in the extremities to more severe manifestations such as pain, muscle weakness, coordination issues, and even organ dysfunction.
While diabetic neuropathy tends to develop over several years, it often goes unnoticed until the nerve damage is substantial enough to trigger noticeable symptoms. This subtle onset underscores the importance of regular check-ups and early diagnosis.
The Importance of Early Diagnosis
 Diabetic neuropathy is often insidious in its onset, with high blood sugar levels slowly damaging the nerves over several years before noticeable symptoms appear. This underscores the importance of early diagnosis and immediate management.
Diabetic neuropathy is often insidious in its onset, with high blood sugar levels slowly damaging the nerves over several years before noticeable symptoms appear. This underscores the importance of early diagnosis and immediate management.
Regular check-ups and blood sugar monitoring are essential for individuals with diabetes. Through these preventive measures, any nerve damage can be caught early. Recognizing the early signs of diabetic neuropathy, such as a loss of sensation, numbness, tingling, or pain in the feet, is crucial. Starting treatment early increases the chances of controlling symptoms and preventing further nerve damage.
The duration it takes for diabetic neuropathy to develop varies depending on individual factors such as the duration of diabetes, how well it’s managed, and individual biological factors. Some may start experiencing symptoms within a few years of a diabetes diagnosis, while others may remain symptom-free for several years.
Treatment Options for Diabetic Neuropathy
Comprehensive View of Treatment Options
The diabetic neuropathy treatment approach is multi-pronged and encompasses slowing disease progression, managing symptoms, and treating any potential complications. The primary focus is on better glucose control to prevent further nerve damage and addressing individual symptoms to improve the patient’s quality of life.
Medication as the First Line of Treatment
Medication serves as the first line of treatment for managing symptoms associated with diabetic neuropathy. Various classes of drugs are available, each with its unique mechanisms of action in relieving the discomfort that neuropathy often brings.
- Anticonvulsants: Drugs like pregabalin and gabapentin, traditionally used for seizure disorders, have been found effective in relieving nerve pain. These medications work by calming hyperactive nerves and are generally well-tolerated by patients.
- Antidepressants: Certain antidepressants interfere with the chemical processes in your brain and spinal cord that make you feel pain, effectively easing the pain caused by diabetic neuropathy. This class includes tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors (SNRIs), and selective serotonin reuptake inhibitors (SSRIs).
- Opioids: For severe pain unresponsive to other medications, opioids may be considered. However, due to their risk of dependency and side effects, they are typically reserved as a last resort.
- Topical Medications: Topical agents such as capsaicin cream or lidocaine patches can be applied directly to the skin where the pain is most severe. They offer localized relief with minimal systemic side effects.
The Role of Physical Therapy
 In some cases, physical therapy can be beneficial. Regular exercises can help improve muscle strength, increase mobility, and manage pain. Specialized therapists can guide patients through a series of exercises designed to meet their specific needs and capabilities.
In some cases, physical therapy can be beneficial. Regular exercises can help improve muscle strength, increase mobility, and manage pain. Specialized therapists can guide patients through a series of exercises designed to meet their specific needs and capabilities.
Interventional Treatments
When symptoms persist despite medication, interventional treatments may become necessary. These treatments provide more direct and often more potent relief by targeting the nervous system directly.
Nerve Blocks
Nerve blocks involve injecting local anesthetics directly into the affected nerves. The anesthetics work by numbing the nerves and blocking the transmission of pain signals to the brain.
In some cases, steroids may also be added to the injections to decrease inflammation and swelling, which can also contribute to pain. Nerve blocks can provide immediate and long-lasting relief for many patients, making them an effective treatment option for those with severe neuropathic pain.
Spinal Cord Stimulation
Spinal cord stimulation is a more advanced interventional treatment where a small device, similar to a pacemaker, is implanted under your skin. The device delivers low-level electrical signals directly to your spinal cord, interfering with the transmission of pain signals to the brain.
Patients can control the intensity of these signals using a handheld remote, allowing them to adjust the level of relief they get. While this procedure requires minor surgery, it can provide significant, long-term relief for patients who haven’t found success with other treatments.
Intravenous Immune Globulin (IVIG) and Plasma Exchange (Plasmapheresis)
For certain types of neuropathy, especially those linked to autoimmune conditions, treatments like intravenous immune globulin (IVIG) and plasma exchange (plasmapheresis) can be beneficial. IVIG treatment involves introducing healthy antibodies into the bloodstream, which can help tame the immune response causing the nerve damage. Plasmapheresis, on the other hand, helps remove harmful antibodies from the blood.
At the Ankle & Foot Centers of America, we believe in exhausting all possible avenues to provide our patients with the relief they need. We offer a wide range of treatments, from medication management to advanced interventional procedures, ensuring we have the tools and expertise to manage even the most stubborn neuropathic pain effectively.
Tailored Approach to Treatment
However, it’s essential to note that medication is not a one-size-full-all solution. Every patient’s response to various treatments differs, with some experiencing side effects or inadequate symptom relief. Consequently, a tailored approach considering each patient’s symptoms, overall health, and response to medication is indispensable.
At the Ankle & Foot Centers of America, we prioritize creating a personalized treatment plan for each of our patients. We take into account all factors, including the type of neuropathy, severity of symptoms, patient’s overall health, and lifestyle. Our team collaborates closely with patients to ensure they receive the most effective treatment and monitors their progress, making necessary adjustments to their treatment plan.

Role of Lifestyle Changes and Prevention
Beyond Medication: Lifestyle Changes
While medication plays a crucial role in managing diabetic neuropathy, lifestyle changes often form the backbone of long-term disease management and prevention of further progression.
Maintaining a balanced diet, rich in fruits, vegetables, lean proteins, and healthy fats can help regulate blood glucose levels and provide the necessary nutrients for nerve health. Regular exercise not only aids in maintaining a healthy weight but also helps regulate blood sugar levels and promotes better circulation, essential for nerve health.
Another critical aspect is blood glucose management. Regular monitoring, appropriate medication, dietary control, and regular exercise play a part in maintaining optimal glucose levels. Effective blood glucose management can slow the progression of neuropathy and even prevent the onset of this condition in people with diabetes.
The Role of Specialized Footwear
Foot care is an often-overlooked aspect of managing diabetic neuropathy. Poor sensation in the feet can lead to injuries that can develop into serious complications if unnoticed. Regular foot checks, proper foot hygiene, and using specialized shoes for diabetic neuropathy can help prevent such issues.
Shoes for diabetic neuropathy are designed to provide extra cushioning and support, reducing the risk of skin breakdown and foot ulcers. They accommodate changes in foot shape caused by neuropathy, reducing pressure points and improving comfort.
At the Ankle & Foot Centers of America, we guide our patients on all aspects of lifestyle changes and preventative measures, including guidance on choosing the right footwear.
Patient Background and Diagnosis
Meet James, a 65-year-old retired teacher with a 10-year history of Type 2 diabetes. He started noticing numbness and a tingling sensation in his feet about a year ago. Initially dismissing it as age-related discomfort, he sought medical help when the numbness increased, and walking became painful. Upon referral to the Ankle & Foot Centers of America, he was diagnosed with diabetic neuropathy.
Personalized Treatment Plan
Our team, devised a comprehensive and personalized treatment plan for James. His treatment regimen included medication to manage his nerve pain, coupled with rigorous blood glucose control measures. The team also recommended lifestyle changes, including diet modifications and a low-impact exercise regimen, to aid in better glucose control and weight management.
James was also educated on foot care, given his reduced foot sensation. He was guided on daily foot checks, maintaining foot hygiene, and choosing the right footwear. He was fitted with shoes specifically designed for diabetic neuropathy, which offered better cushioning and accommodated the changes in foot shape caused by neuropathy.
Outcome and Follow-up
Over the following months, James reported a significant reduction in his foot pain, better glycemic control, and improved quality of life. This case illustrates the effectiveness of our comprehensive approach to diabetic neuropathy management and our unwavering dedication to our patients’ health.
Conclusion
Diabetic neuropathy is a complex, chronic condition that requires expert care and comprehensive management. At the Ankle & Foot Centers of America, we understand the intricacies of this condition. Our expertise lies in providing targeted, individualized care—whether that involves prescribing the best diabetic neuropathy medications, advising on lifestyle changes, or recommending shoes for diabetic neuropathy.
Our mission extends beyond providing treatments. We aim to empower patients with knowledge about their condition and involve them in decision-making. This way, we ensure that every patient becomes an active participant in their healthcare journey.
To our fellow medical professionals, we extend our commitment to collaborative care. We believe in synergistic partnerships that allow us to provide the best care for our patients. By sharing knowledge and resources, we can better serve those suffering from diabetic neuropathy.
Living with diabetic neuropathy can be challenging. But with the right help and guidance, it’s possible to manage the condition effectively and lead a fulfilling life. At the Ankle & Foot Centers of America, we’re dedicated to making this possible.